Article Topics
 Recently, the American Nurses Association (ANA) came out with a statement declaring their acknowledgement of cannabis as medically beneficial, and asking the federal government to reschedule cannabis for the purpose of furthering medical studies. This may seem like a major revelation, unless you’re aware that the ANA has been advocating for the rescheduling of cannabis since 1996.
Recently, the American Nurses Association (ANA) came out with a statement declaring their acknowledgement of cannabis as medically beneficial, and asking the federal government to reschedule cannabis for the purpose of furthering medical studies. This may seem like a major revelation, unless you’re aware that the ANA has been advocating for the rescheduling of cannabis since 1996.
A Twenty-Year History of Nurses Advocating for Cannabis
In the 1990’s, the endocannabinoid system was discovered, and the health benefits associated with the combining of the two became evident. Because the body has natural receptors to cannabinoids, ingesting cannabis has a wealth of benefits. The ANA holds that “Marijuana has been used for alleviating symptoms of nausea and vomiting; stimulating appetite in HIV patients; alleviating chronic pain; easing spasticity due to multiple sclerosis; decreasing symptoms of depression, anxiety, sleep disorders and psychosis; and relieving intraocular pressure from glaucoma.”
However, at the federal level cannabis is classified as a Schedule I substance, which designates the plant as having no medicinal value. Because of this, it is increasingly difficult to study cannabis, even in decriminalized states. In order to study cannabis, scientists must first obtain a Schedule I research license, and can only receive specimens from the National Institute on Drug Abuse (NIDA). NIDA is currently the only institution that is legitimately permitted to study marijuana, but their motivations (studying drug abuse but not the benefits of cannabis) are contradictory to those of pro-cannabis health professionals.
In the full statement, the ANA reiterates its 1996 stance that “Marijuana and its derivatives continue to be used to alleviate disease-related symptoms and side effects.” However, they also concede that, due to current federal regulations, “findings of anecdotal and controlled studies regarding the efficacy for patient use are mixed.” The 2016 ANA position statement is a stark reminder that for 20 years, health workers have been asking the federal government to amend the scheduling of cannabis so that its health benefits can be fully analyzed.
symptoms and side effects.” However, they also concede that, due to current federal regulations, “findings of anecdotal and controlled studies regarding the efficacy for patient use are mixed.” The 2016 ANA position statement is a stark reminder that for 20 years, health workers have been asking the federal government to amend the scheduling of cannabis so that its health benefits can be fully analyzed.
And it’s not just about research. It’s about lifting the stigma and getting the federal government on the same page as half the states. The fact that there are opposing laws on the state and federal level means that we’re left floundering in an uncomfortable gray area when it comes to liability. Both patients and health workers alike face potential legal action from the federal government for the use or prescription of legal marijuana. Because of this, many patients shy away from the medicine they need, and health workers become timid about expanding their health knowledge to include cannabis.
Eloise Theisen, a nurse and longtime advocate of medical marijuana describes the dire need for rescheduling. She notes that, because of the current classification, health care professionals don’t receive training on the endocannabinoid system. Therefore, most nurses or doctors would be unable to provide effective advice for the use of marijuana for medicinal purposes. Instead, she points out, patients who want to use medical marijuana must seek advice from dispensary workers who are not medically trained. Because there is no official training, and little research, advice often varies from dispensary to dispensary.
 “Cannabis is medicine and needs to be treated as such. Nurses are on the front lines and recognize that our patients are using it. As educators and advocates, nurses deserve to be trained on cannabis medicine so they can help their patients receive maximum benefit. Training is severely lacking and many organizations are still burying their heads in the sand.”
“Cannabis is medicine and needs to be treated as such. Nurses are on the front lines and recognize that our patients are using it. As educators and advocates, nurses deserve to be trained on cannabis medicine so they can help their patients receive maximum benefit. Training is severely lacking and many organizations are still burying their heads in the sand.”
There are plenty of patients out there who are experiencing ineffective pharmaceuticals or pharmaceuticals that have too many side-effects, and want to find an alternative. Sometimes patients just want an addendum to the medications they’re taking. For example, if a cancer patient is undergoing chemotherapy and is facing difficulty eating, they may want to start using cannabis as a way to boost their appetite. But without proper knowledge of dosage, strain, or administration, finding an alternative or a medical addition in cannabis can become frustrating. Many patients have to scour endless pages of research, and attempt a trial and error administration.
Stigma, Shame and Lack of Education Impacts Cannabis Education
Plus, the stigma of using marijuana is strong. “When UPG and GHC partnered to bring training to nurses in CA, the board of registered nursing failed to approve the content for contact hours that can be used toward license renewal,” says Eloise Theisen. “I followed all of the steps in plenty of time and was told that I needed to provide more scientific research as to why this content is relevant to the practice of nursing. Even after providing that, the BRN (Board of Registered Nursing) has not approved the request to provide the content and it continues to be under review.”
Patients who wish to use cannabis as a supplement to the medication they’re already taking may balk at asking their health care professionals for advice out of fear of shame or rejection. Although cannabis is one of the safest medicines out there, there is still a possibility of negative drug interactions. That’s why it’s imperative that health care professionals know the material and patients feel safe asking.
United Patients Group and Nurses – Education in Action
To address this issue, United Patients Group, kicked off their second annual cannabis conference this year, including a nurse’s training program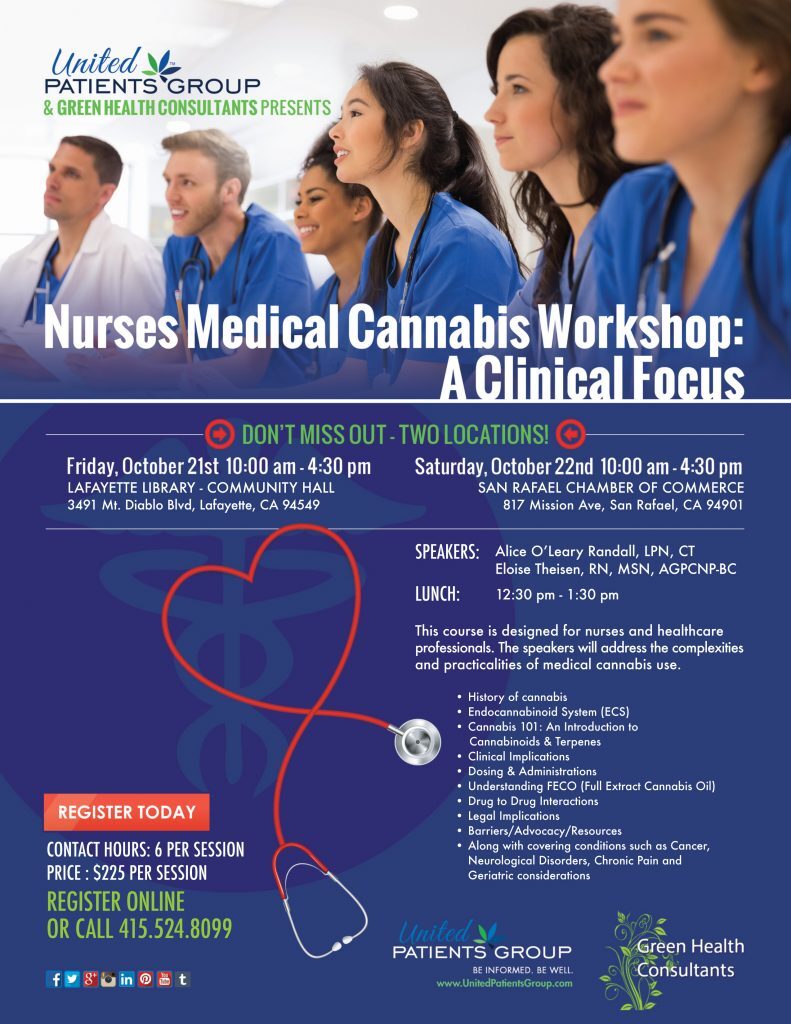 . The conference featured presentations by experts in the field as well as patients-turned-advocates who have benefited from medical marijuana. The conference seeks to expel myths and present the science behind medical marijuana.
. The conference featured presentations by experts in the field as well as patients-turned-advocates who have benefited from medical marijuana. The conference seeks to expel myths and present the science behind medical marijuana.
During the nurse’s training course, attendees came from all over the world to learn about the endocannabinoid system, legal issues, dosing, full extract cannabis oil, how to talk to their employers about incorporating cannabis into their treatment plans, drug interactions, and more.
As one of the speakers at the conference, Eloise Theisen shared her knowledge of medical cannabis and discussed where she would like to see the future of the industry.
More recently, United Patients Group hosted a full weekend of education for nurses in Northern California. Again, the program was sold out, and the obvious interest in, and need for, accredited training for medical professionals was clear.
“We have plenty of research on cannabis in animals and now we are seeing a lot of observational data come out from those who are working in the field of cannabinoid medicine. Personally, I would like to see more research on drug-drug interactions with cannabis as well as bio availability rates among different delivery methods,” Theisen commented.
It’s very telling that the BRN does not accept medical marijuana training as a legitimate course for license renewal despite the evidence, and despite the ANA’s stance on the legalization of marijuana. But the climate is changing rapidly with more states legalizing cannabis, and the continued advocacy by the ANA, training offered by UPG, and experts such as Eloise Theisen and Alice O’Leary Randall. We may one day soon see medical professionals getting the training they need and patients receiving the treatment they deserve.